It’s Thursday night, 00:11 AM. Purva receives a notification on her phone, that the Catharina hospital in Eindhoven has just reported a donor. Working the night shift at Eurotransplant, she can start the allocation process for the 64-year-old male donor, who was declared brain dead two hours ago.
Purva swiftly runs the match procedure for the liver and the kidneys. These organs were deemed suitable for transplantation by the Catharina hospital. She is informed that the explantation procedure is scheduled for 08:00 AM, which means that Purva has just under 8 hours to find candidates for transplantation. Within minutes, Purva has printed out a list of candidates eligible to receive the organs, and picks up the phone to call a hospital in Vienna; the candidate listed there has a High Urgency (HU) status, and is likely to die within days if not transplanted.
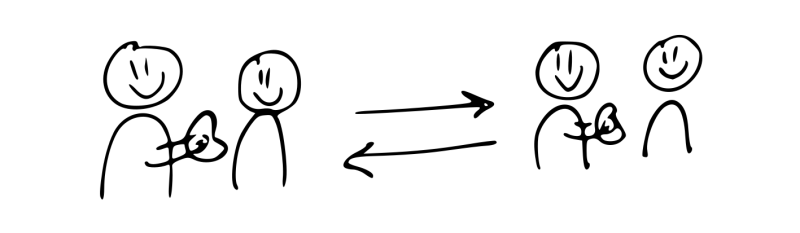
The scenario above is not unique: every year 2000 deceased organ donors from eight European countries are reported to Eurotransplant. Eurotransplant staff offers the available organs to transplantation candidates, who are registered on organ-specific waitlists. Purva could start offering the liver to transplant candidates within mere minutes thanks to Eurotransplant’s liver match algorithm. Based on the waiting list and candidate and donor characteristics, this algorithm puts out a list of all candidates eligible for liver transplantation, ranked in terms of priority for the liver offer.
Top priority was given to the Viennese candidate, whose High Urgency status indicates they are expected to die within 7 days if not transplanted. After some deliberation, the Viennese donor coordinator tells Purva that they have to decline the liver offer: their patient is currently medically unstable. Purva moves on to offer the liver to a 2-year old patient in Groningen. Groningen’s duty officer also turns down the offer, deeming the donor too old for transplantation into the 2-year old child.
Ranks 3 through 5 are occupied by Dutch adult patients, listed in Rotterdam and Leiden. The ranking of these patients was determined by their so-called MELD scores. The higher the MELD score, the more likely a candidate is to die within three months if no transplant is received. The candidates have MELD scores of 31, 28, and 27, respectively. These correspond to 90-day mortality risks of 55%, 42% and 38%, respectively (in absence of transplantation).
Rotterdam considers the liver physically too large for the female patients at rank 3 and 4, and turns down the liver offer. Eventually, the liver is accepted for transplantation into the 5th ranked candidate, a male patient listed in Leiden University Medical Center (LUMC).
Having placed the liver graft, Purva moves on to allocate the donor’s kidneys.
Medical urgency as the cornerstone of Eurotransplant liver matching algorithm
Purva’s swift matching of the donor’s liver to the candidate in Leiden was facilitated by Eurotransplant’s match list algorithm. This algorithm considers dozens of factors to rank candidates who await a liver transplantation. These factors range from medical requirements such as blood group compatibility, to ethical considerations such as priority for children. Of paramount importance for the liver algorithm is the medical urgency of a candidate.
This medical urgency is quantified with MELD scores, which are calculated based on three biomarkers measured from blood samples of candidates: serum creatinine, serum bilirubin, and the INR. Centers have to report these biomarkers periodically for their liver transplantation candidates to Eurotransplant. MELD does not fully determine the prioritization of patients, but it plays an important role. In the example above, the three adult patients in Rotterdam and Leiden were ranked in order of descending MELD scores. With this prioritization scheme, Eurotransplant tries to help the sickest patients first.
The precarious position of females in liver allocation
Unfortunately, persistent donor shortages mean that not all transplantation candidates can be helped in time. In fact, nearly 400 transplant candidates die every year within Eurotransplant while waiting for a liver transplantation.
A fairness issue is that female patients are overrepresented among this group: in Eurotransplant, an average of 7.8% of females die within 90 days after listing, compared to 6.7% of males. Moreover, fewer females receive a transplantation, with 22% of females transplanted 90 days after listing, compared to 29% of males. These sex disparities exist despite the fact that males and females have similar MELD scores at listing.
In the medical literature, two explanations have been proposed for this precarious position of females in liver allocation. The dominant explanation is that MELD’s use of serum creatinine makes it inherently biased against females, because females have inherently lower serum creatinine than males. The other explanation is that females have to 'reject' a liver more often than males. A liver has to fit in the abdominal cavity of the transplant recipient, and has to meet the recipient’s metabolic needs. Typically, females have a smaller stature than males, making it more difficult to find an appropriately-sized liver. Often, a liver is simply too big. This extends waiting time, which exposes the patient to a higher risk of a waitlist death.
Several alternatives to MELD have been proposed which aim to rectify such sex disparity, typically by giving extra points to female candidates. One example of such a score is MELD 3.0, which has been used in the United States for liver allocation since 2023, which gives 1.3 extra points to female candidates.
First, let us look at how MELD 3.0 reduces sex disparity. Then, let's look at why this system does not suffice to completely fix the problem.
The hazard ratio as the basis for extra MELD points for female patients
MELD 3.0 gives 1.3 extra points to female candidates. These 1.3 extra points originate from a Cox proportional hazards model which suggests that females have a significantly higher mortality hazard rate than males with the same MELD score. The mortality hazard rate is the rate at which patients die after having been on the waitlist for a given amount of time  .
.
The Cox proportional hazards model, often used by medical researches, makes important assumptions on the mortality hazard rate. In our case, it assumes that the mortality hazard rate of females is the mortality hazard rate of males multiplied by some factor. We call this multiplication factor the hazard ratio.
If the hazard ratio exceeds 1, this indicates that female patients face inherently higher pre-transplant mortality rates than males when at the same MELD score. In the United States, the hazard ratio was estimated to be approximately 1.27, which led to 1.3 extra points for female candidates being awarded for MELD 3.0. As a a result, females are ranked higher than before wherever MELD determines the ranking. Hence, females receive transplants more often and the sex disparity decreases. Unfortunately, this is not the full story.
Why MELD 3.0 may not necessarily fix sex disparity in waitlist outcomes
Using MELD 3.0 thus ensures that the mortality hazard rate of females is fairly estimated. Sadly, it is often overlooked that replacing MELD by MELD 3.0 is not sufficient to remove all sex disparity in waiting list outcomes.
It is helpful to illustrate this with a realistic statistical simulation. For this simulation, we simulate 10 years of data for 17 000 liver transplantation candidates. In these simulations, females have an inherently higher waitlist mortality hazard rate than males, as is the case in reality. We let this disadvantage correspond to 1.3 points on the MELD scale. We prioritize candidates for transplantation based on MELD 3.0 score, which awards females these 1.3 extra points. The crux is that is insufficient to rectify sex disparities in waitlist outcomes.
The reason why sex disparity persists is that shorter candidates are simulated to be less likely to accept an accepted liver graft. With females simulated to be 15 cm shorter on average, they need to turn down more offers, spend more time at risk of a waitlist death, and consequently pass away more often on the waiting list.
Simulating liver allocation
We generate MELD scores, candidate sex, the candidate’s blood group, and the candidate’s country of listing from their observed data of Eurotransplant. This ensures that our simulated candidate population closely matches the real candidate population. We also simulate a height for each candidate, with female height on average 15cm lower than male height. We simulate a candidate’s survival in the absence of transplantation according to the Cox proportional hazards model described before. This means that females face 23% higher waitlist mortality rates than males when at the same MELD score. This then corresponds approximately to a  point difference on the MELD scale.
point difference on the MELD scale.
Importantly, we also the offer acceptance or denial of a liver. This is partly based on the candidate's MELD score and their height (smaller candidates cannot accept large livers, because of size mismatch), but there is also a random component.
For candidates, we assume that 1200 candidates were on the waiting list at the simulation start date, and that the other candidates’ registration times were uniformly distributed over the ten years of simulation. We assume that livers become available for allocation from  donors, who are reported uniformly at random over the total time of the simulation. Donor countries and blood groups are simulated to match those of Eurotransplant’s actual donor population.
donors, who are reported uniformly at random over the total time of the simulation. Donor countries and blood groups are simulated to match those of Eurotransplant’s actual donor population.
In the simulation, we offer the donors to candidates with an active waitlist registration. In these simulations, offers are only made within the same blood group and within the same country. We rank candidates by their MELD 3.0 score. Candidate acceptance behavior is simulated according to the model outlined above. For candidates who accepted a liver offer while they have an active waitlist registration, we record a transplantation. For candidates who were simulated to die before accepting a liver offer, we record a waitlist death.
Simulation result: sex disparity goes unnoticed by the MELD 3.0 model
After 10 years of simulation, we find stark sex disparity in waitlist outcomes: 9.3% of females have died 90 days after listing, compared to 6.1% of males. Regarding transplantations, we find that 35% of females were transplanted 90 days after listing, compared to 43% of males.
To correct this sex disparity, one could try to develop a new score by estimating the hazard ratio for female sex, and giving extra points to rectify the remaining disparity. How many extra points would it give to females? As it turns out, none.
This may appear surprising, because relatively more females have died on the waiting list than males. This tells us that the Cox proportional hazards model cannot be used in this way to fully rectify sex disparity in waiting list outcomes.
What more can be done to resolve sex disparities in waitlist outcomes
What does this simulation tell us? First, note that the simulation is a heavily simplified representation of the liver allocation process. For example, we have ignored that patients routinely update their MELD scores, as well as all most factors considered in allocation by Eurotransplant’s liver matching algorithm.
Still, main point of the simulations is that sex disparities can still arise in waiting list outcomes, even when allocation is based on an unbiased estimate of the waiting list mortality hazard rate faced by male and female candidates (e.g., MELD 3.0). In our simulations, these disparities arose because female candidates were 25% less likely to accept an organ offer than male candidates. These lower acceptance rates were not necessarily caused by female sex, but rather by the fact that females tend to be shorter than males. To rectify this sex disparity, one should think of other approaches, such as giving small-statured candidates extra priority to small donor livers.
Does this mean that MELD 3.0 is a failure? Preliminary findings suggest that MELD3.0 has the potential to reduce sex-based disparities in liver transplant opportunities and waitlist mortality. To conclude, while MELD 3.0 can serve as a step towards decreasing sex disparity in liver allocation, research into extended or other approaches for resolving sex disparity in liver allocation is needed.
Cover photo was taken from the Happiest Health website.